Big Data in Healthcare: Revolutionizing Patient Care
Introduction
In the rapidly evolving landscape of healthcare, big data has emerged as a transformative force, enabling unprecedented insights into patient care, disease management, and operational efficiency. Defined by its volume, variety, velocity, and veracity, big data encompasses vast datasets from electronic health records (EHRs), wearables, genomic sequencing, and more, generating over 2,314 exabytes daily by 2025. This chapter explores how big data is revolutionizing patient care, from predictive analytics to personalized medicine, while addressing benefits, challenges, and future trends. As of 2025, integrations of artificial intelligence (AI) and big data analytics are not only improving outcomes but also bridging gaps in access, with AI expected to accelerate markets like traditional, complementary, and integrative medicine (TCIM) to nearly $600 billion.
Sources of Big Data in Healthcare
Big data in healthcare draws from diverse sources, creating a rich ecosystem for analysis:
- Electronic Health Records (EHRs): Comprehensive patient histories, including diagnoses, treatments, and outcomes.
- Wearable Devices and IoT: Real-time data from smartwatches, fitness trackers, and sensors monitoring vital signs like heart rate and glucose levels.
- Genomic and Molecular Data: Sequencing results providing insights into genetic predispositions.
- Diagnostic Imaging and Lab Results: High-volume data from MRIs, CT scans, and blood tests.
- Administrative and Claims Data: Billing, insurance, and operational records for fraud detection and resource allocation.
- Social Determinants of Health: External data on lifestyle, environment, and socioeconomic factors.
By 2025, advancements like the European Health Data Space (EHDS), effective March 26, 2025, standardize data sharing across EU countries, enhancing interoperability. Cloud computing and blockchain further enable secure, scalable access, supporting real-time collaboration.
Key Applications of Big Data in Healthcare
Big data applications are reshaping healthcare delivery through innovative uses:
- Predictive Analytics for Disease Prevention: Analyzes EHRs, wearables, and genetics to forecast risks. For instance, Kaiser Permanente's PREVENT tool assesses cardiovascular risks, reducing severe issues by up to 72% via personalized plans. In 2025, tools like FaceAge improve cancer survival predictions from 61% to 80% using facial features.
- Personalized Medicine: Tailors treatments using genomic and lifestyle data. Mayo Clinic applies this in breast cancer for customized therapies. Queen's University Belfast, in January 2025, combined clinical and genomic data for prostate cancer plans.
- Hospital Operations Optimization: Optimizes workflows and resources. Cleveland Clinic uses AI for nurse scheduling, reducing wait times. In August 2025, Cleveland Clinic and Piramidal developed an AI model for ICU brain monitoring, cutting detection times.
- Population Health Management: Aggregates data for disparities and interventions. The UK's NHS uses linked datasets for vaccination campaigns. Northwell Health monitors trends for community needs.
- Drug Discovery and Development: Accelerates trials with clinical and genomic data. Pfizer uses AI for cystic fibrosis therapies. Oxford Drug Discovery Institute, in April 2025, streamlined Alzheimer's research.
- Remote Monitoring and Telemedicine: Wearables enable real-time care. Kaiser Permanente integrates this for chronic diseases.
- Fraud Detection: Identifies irregularities in claims. UnitedHealth Group reduces waste with predictive modeling.
These applications, enhanced by AI, achieve diagnostic accuracies up to 94% for eye diseases and 30% earlier cancer detection.
Benefits of Big Data in Healthcare
The integration of big data yields substantial advantages:
- Improved Patient Outcomes: Early interventions and personalized care reduce mortality and complications. Predictive tools decrease readmissions by 15% and ER overcrowding by 40%.
- Cost Reduction: Optimizes resources, cutting operational inefficiencies. Hospitals report 25% fewer surgery delays and 30% shorter wait times.
- Health Equity: Targets underserved populations, reducing disparities via telehealth and mobile clinics.
- Operational Efficiency: Streamlines workflows, with AI forecasting improving staff allocation.
- Research Acceleration: Speeds drug development, as seen in Pfizer's ML models reducing timelines.
- Fraud Prevention: Saves billions, with AI detecting $1.3 billion in fraudulent claims.
Overall, big data shifts healthcare from reactive to proactive, enhancing precision and accessibility.
Challenges and Ethical Considerations
Despite its potential, big data faces hurdles:
- Data Privacy and Security: Sensitive information requires HIPAA compliance; breaches are costly.
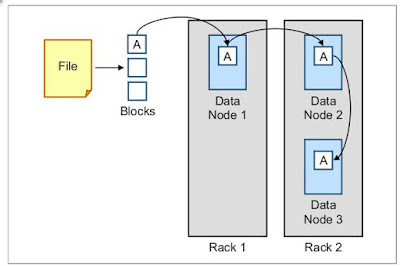
- Integration and Interoperability: Siloed systems hinder sharing; standards like HL7 FHIR help but are inconsistent.
- Data Quality and Standardization: Incomplete or varied data affects analysis.
- Skill Gaps: Need for data-savvy professionals; programs like those at MGH Institute address this.
- Ethical Issues: Bias in AI and equitable access must be managed.
Regional computing paradigms, like proposed frameworks for healthcare big data (HBD), aim to mitigate these via localized servers.
Case Studies
Real-world implementations illustrate big data's impact:
- UCSF Health & GE Healthcare: Predictive analytics reduced ICU mortality and stay using ML and EHRs.
- Massachusetts General Hospital: Optimized operations with queuing theory, cutting wait times and costs.
- Kaiser Permanente & IBM Watson Health: Managed population health, reducing hospitalizations via predictive tools.
- Cleveland Clinic: Reduced medication errors with NLP and real-time support.
- Memorial Sloan Kettering & Flatiron Health: Personalized cancer care with genomic data, improving responses.
- BenevolentAI (Drug Discovery): Identified COVID-19 treatment baricitinib rapidly using AI and cloud.
- GlaxoSmithKline (Clinical Trials): Unified data lake cut query times from a year to 30 minutes.
- Pfizer (Manufacturing): Predictive maintenance via IoT reduced downtime.
- Geisinger Health System: AI for early detection and care coordination in value-based models.
- Omada Health: Data-powered coaching for chronic care, enhancing coordination.
These cases demonstrate tangible improvements in efficiency and outcomes.
Future Trends
Looking ahead, trends include:
- AI and ML Integration: Large language models (LLMs) for medical AI, revolutionizing diagnostics.
- Digital Twins and Blockchain: Virtual patient models and secure data sharing.
- Expanded Wearables: Real-time insights via IoT.
- Global Data Spaces: Like EHDS, fostering collaboration.
- Ethical AI Focus: Addressing biases for equitable care.
By 2025, expect more AI-powered forecasting and personalized tools.
Conclusion
Big data is fundamentally revolutionizing healthcare, driving personalized, efficient, and equitable patient care. While challenges persist, ongoing innovations promise a future where data empowers better health for all. As integrations deepen, the potential to transform outcomes and reduce costs will only grow, marking a new era in medicine.



Comments
Post a Comment